Healthcare practices today face the challenge of managing patients with complex chronic conditions while maintaining efficiency and revenue. While Chronic Care Management (CCM) addresses patients with two or more chronic conditions, many patients have one high-risk condition that still requires intensive, ongoing support.
That’s where Principal Care Management (PCM) comes in.
PCM Meaning in Healthcare
What does PCM stand for in medical terms?
PCM means Principal Care Management. It is a Medicare-recognized care management program designed for patients with one complex chronic condition expected to last at least 3 months and that significantly impacts their daily life or health outcomes.
In medical terms, PCM services include:
- Care plan development
- Medication management
- Patient education
- Monthly care coordination outside of face-to-face visits
PCM in healthcare ensures patients with one serious chronic condition — like COPD, cancer, diabetes, or advanced heart disease — receive structured support between office visits.
PCM vs CCM: What’s the Difference?
A common question: what is the difference between PCM and CCM?
- CCM (Chronic Care Management): For patients with two or more chronic conditions. CPT codes include 99490, 99439, 99491, etc.
- PCM (Principal Care Management): For patients with one high-risk chronic condition that demands ongoing monitoring. PCM CPT codes include 99426 and 99427.
In short: CCM = multiple conditions; PCM = one principal condition.
“…PCM is one of four Care Management Solutions recognized by Medicare.”
99426 CPT Code Description & Billing Guidelines
The most commonly used code for PCM is 99426.
- 99426 CPT code description: Principal Care Management, 30 minutes of clinical staff time per month, directed by a physician or other qualified healthcare professional (QHP).
99427 CPT code: Each additional 30 minutes of staff time in the same month.
Principal Care Management Billing Guidelines
- Patient eligibility: One chronic condition lasting ≥3 months with significant health risk.
- Time tracking: At least 30 minutes of non-face-to-face PCM services each month.
- Consent: Document informed consent for PCM enrollment.
- Care plan: Must include diagnosis, treatment, goals, and monitoring.
- No overlap: Time billed under 99426/99427 cannot be double-counted with CCM, BHI, or RPM.
Related: Principal Care Management Billing vs CCM Billing
Benefits of PCM in Healthcare
For Patients
- Ongoing support for a serious chronic condition.
- Better treatment adherence.
- Reduced hospitalizations.
- More trust and engagement with providers.
For Providers
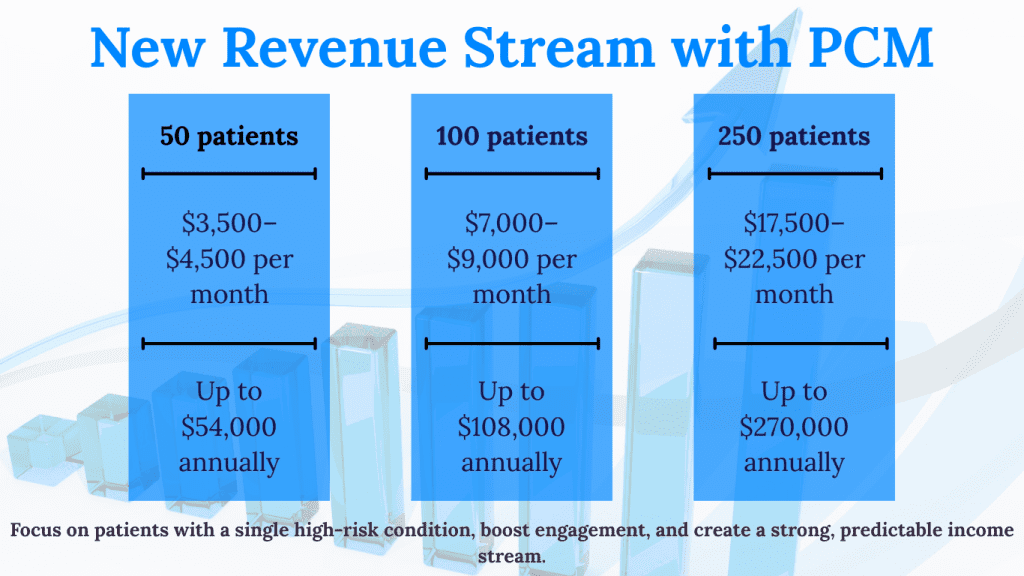
- New revenue stream from PCM CPT codes.
- Improved patient retention and outcomes.
- Flexibility to transition patients into CCM or BHI when they qualify.
- Stronger performance under value-based care models.
Revenue Example:
A primary care practice enrolling 150 patients in PCM billing (99426) could generate $14,000/month in recurring revenue.
PCM Services: What’s Included?
PCM services are designed to ensure comprehensive management of one serious chronic condition. They include:
- Developing and updating a care plan
- Medication reconciliation and adherence checks
- Patient and caregiver education
- Care coordination with specialists or hospitals
- Monitoring patient progress and making necessary adjustments
By delivering these PCM services, practices provide high-quality care and meet CMS billing requirements.
Common PCM FAQs
Q1: What is PCM in medical terms?
PCM = Principal Care Management, a CMS program for managing one serious chronic condition.
Q2: What is the 99426 CPT code?
99426 is the primary CPT code for PCM, covering the first 30 minutes of monthly clinical staff time.
Q3: What other PCM CPT codes exist?
99427 covers each additional 30 minutes in the same month.
Q4: What conditions qualify for PCM?
Examples: COPD, advanced cancer, CHF, severe diabetes.
Q5: What are PCM services?
Services include care planning, education, medication management, coordination, and monthly patient engagement.
PCM in Action: Success Story
A cardiology clinic implemented PCM services for heart failure patients:
- Enrolled 80 patients in 99426 billing.
- Reduced hospital readmissions by 22%.
- Generated $7,500/month in PCM reimbursement.
Improved patient adherence to prescribed care plans.
CareNova: Your Partner in Principal Care Management
Launching a PCM program can be complex. CareNova provides:
- Turnkey PCM implementation (EHR integration, billing workflows).
- Staff training on 99426/99427 billing guidelines.
- Patient onboarding systems for smooth enrollment.
Compliance oversight to ensure maximum reimbursement.
Final Thoughts: Why PCM Is a Growth Lever
Principal Care Management (PCM) is one of the most underutilized Medicare programs — yet it represents a powerful way for practices to increase revenue, improve outcomes, and deliver patient-centered care.
At CareNova, we specialize in helping practices implement PCM services that align with compliance and value-based care goals.
Schedule a Free Consultation with CareNova Today to unlock new PCM revenue opportunities in your practice.



