Introduction — What Is Chronic Care Management?
Chronic Care Management (CCM) is a Medicare-covered service designed for patients with two or more chronic conditions expected to last at least 12 months or until death.
It focuses on making and keeping track of a full care plan, making sure that follow-up is consistent, getting people to take their medications as prescribed, and lowering the number of hospitalizations.
What Conditions Qualify for Chronic Care Management?
Studies from the National Institutes of Health show CCM programs significantly improve patient outcomes while lowering healthcare costs.
Medicare defines qualifying chronic conditions as those that place the patient at significant risk of death, acute exacerbation, or functional decline.
Common qualifying conditions include:
- Diabetes
- Hypertension
- Chronic Obstructive Pulmonary Disease (COPD)
- Heart disease
- Arthritis
- Depression
- Chronic kidney disease
Explore about our Remote Patient Management services .
Chronic Care Management CPT Codes Explained
Correct coding is the foundation of Medicare compliance and maximizing reimbursement.
99490 CPT Code Description
Covers the first 20 minutes of non-face-to-face clinical staff time per patient per month. Requires a documented care plan and patient consent.
99439 CPT Code Description
An add-on code for each additional 20 minutes of non-face-to-face care provided in the same month.
Why these matter: Correctly applying chronic care management CPT codes ensures full capture of revenue while meeting compliance requirements.
Medicare Physician Fee Schedule for Chronic Care Management
Medicare reimbursement is calculated using:
- CPT billing codes
- Relative Value Units (RVU) for the service
- Conversion Factor (CF) — national dollar multiplier
- Geographic Practice Cost Index (GPCI) — adjusts for local costs
2025 National Average Medicare Rates
(Estimates, subject to 2026 updates — see CMS Physician Fee Schedule):
| CPT Code | Description | Avg. Reimbursement (2025) |
| 99490 | Initial 20 minutes CCM | $62.50 |
| 99439 | Additional 20 minutes CCM | $47.50 |
2026 Outlook: CMS may adjust conversion factors and introduce new chronic care management billing guidelines to reduce administrative burden and improve payment efficiency.
How a Chronic Care Management Program Works
A successful Medicare chronic care management program typically includes:
- Patient Enrollment — Identifying eligible Medicare patients and obtaining consent.
- Care Plan Creation — Developing comprehensive, patient-centered care plans in the EHR.
- Monthly Check-ins — Calls or telehealth visits to review progress, update care plans, and address patient concerns.
- Ongoing Coordination — Communicating with specialists, pharmacies, and labs to keep care aligned.
- Billing & Compliance — Accurate coding for 99490 CPT code and 99439 CPT code to meet Medicare guidelines.
Chronic Care Management Software — Features to Look For
While CareNova does not sell software, we help practices select and implement tools that make CCM more efficient and compliant.
Key features to look for include:
- Automated time tracking for CPT codes
- HIPAA-compliant communication tools (U.S. Department of Health & Human Services HIPAA Overview)
- Patient engagement dashboards
- Reporting tools for Medicare audits
Top Chronic Care Management Companies
Leading providers known for delivering results include:
- CareNova — End-to-end CCM and RPM program implementation with expert Medicare billing compliance support.
- ChartSpan — National CCM provider with strong patient engagement tools.
- HealthSnap — Combined CCM and remote patient monitoring services.
- Prevounce — Compliance-focused CCM program solutions.
- Medsien — Scalable CCM programs for larger practices.
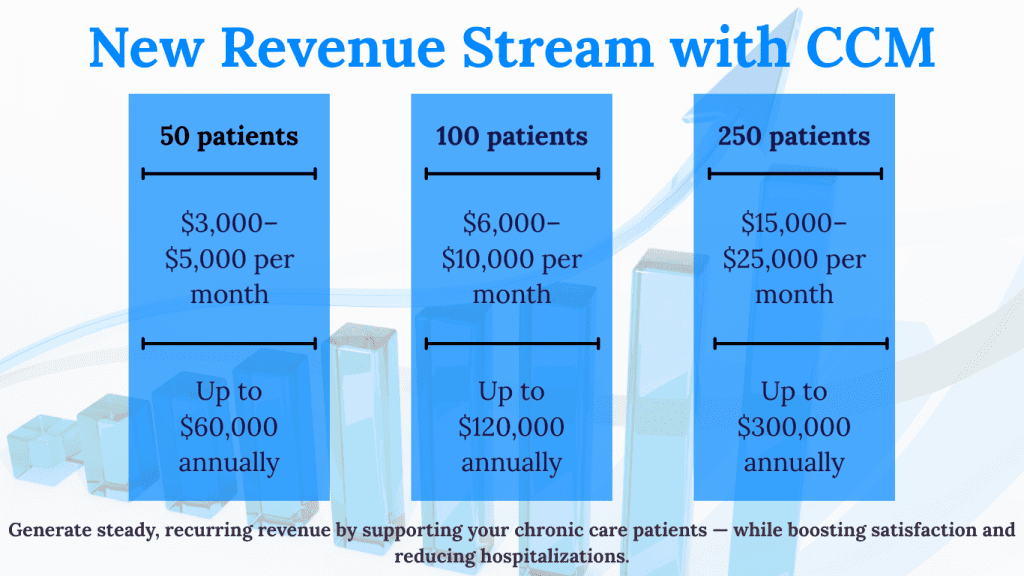
Chronic Care Management Revenue & Patient Care Impact — Real Example
Example: A 500-patient primary care clinic implements a CCM program.
- Enrollment: 120 Medicare patients qualify.
- Revenue Impact: At $62.50 for 99490 + $47.50 for 99439, monthly recurring revenue exceeds $9,000.
- Clinical Impact: Reduced ER visits by 18% in 6 months due to better medication adherence and follow-up care.
Why Partner with CareNova for CCM
We help practices launch and scale CCM programs with:
- Expert Medicare billing compliance
- End-to-end program setup & patient enrollment
- Integrated workflow solutions for efficiency
- Proven track record of boosting both patient outcomes and revenue
→ Contact CareNova to start your CCM program and unlock new recurring revenue streams.
RPM is just one piece of Care Management Solutions
FAQs
Q1: What is chronic care management?
A Medicare-covered service for patients with two or more chronic conditions, focused on care coordination and ongoing patient engagement.
Q2: How much does Medicare pay for CCM?
In 2025, the average national reimbursement is $62.50 for CPT 99490 and $47.50 for CPT 99439.
Q3: What conditions qualify for CCM?
Conditions like diabetes, hypertension, COPD, heart disease, arthritis, depression, and chronic kidney disease qualify.
Q4: Which CPT codes are used for CCM?
The most common are 99490 for the first 20 minutes and 99439 for each additional 20 minutes of care.
Q5: What are the chronic care management billing guidelines for 2026?
CMS is expected to streamline documentation, adjust reimbursement rates, and potentially introduce new billing codes to improve program adoption.
→ CCM is central to Care Management Solutions for practices
→ Adding Remote Patient Monitoring strengthens your CCM program
→ Compare PCM vs CCM billing to choose the right program
→ Integrating CCM with Behavioral Health Integration improves outcomes



